Baby Boomer Mortality Experience: Welcome to Old Age! 2020-2021 U.S. Mortality Increase for Ages 60-79 was Mostly COVID
Over two-thirds of mortality increase was COVID, about 5-10% was from heart disease
Continuing the march through the generations,
So here’s the good news as we move to the senior groups — the relative effect of the pandemic has not been as harsh on the Baby Boomers as it was on the Millennials and Gen Xers.
As noted in the previous posts, one of the reasons for the very high increase in overall mortality for young adults and middle-aged adults was that both drug overdoses and COVID had large effects in those age groups. So the peak age group affected, age 40-44, had an over 50% increase in mortality from 2019 to 2021.
As we see above, the increase for the Baby Boomer groups “only” saw an increase of about 20% to 28%. Yes, that’s still very high. But it’s not 50%.
At these old ages, drug overdoses weren’t as much a factor. Indeed, I had to change what causes of death I looked at below. I had to switch out drug overdoses, and included falls instead for the accidental deaths, as this is more of a factor in accidental deaths for older adults.
Here are my top-level results for Baby Boomer mortality results in 2020-2021:
Over two-thirds of the increase of mortality for ages 60-79 in both 2020 and 2021 came from COVID.
The second-most “rankable” reason for increased mortality was heart disease, but the percentage attribution was at a much lower magnitude — ranging from 5% – 11% of the cause.
Chronic lower respiratory disease provided a negative contribution to mortality in both years for ages 60-79 — that is, there was a lower rate for this cause of death in both 2020 and 2021.
Cancer death rates were lower in 2020 for ages 60-79, but it was mixed in 2021. It was lower for ages 60-64, and higher for ages 65-79 in 2021.
Below I will share graphs from each age group and some observations for each age group.
Age 60-64
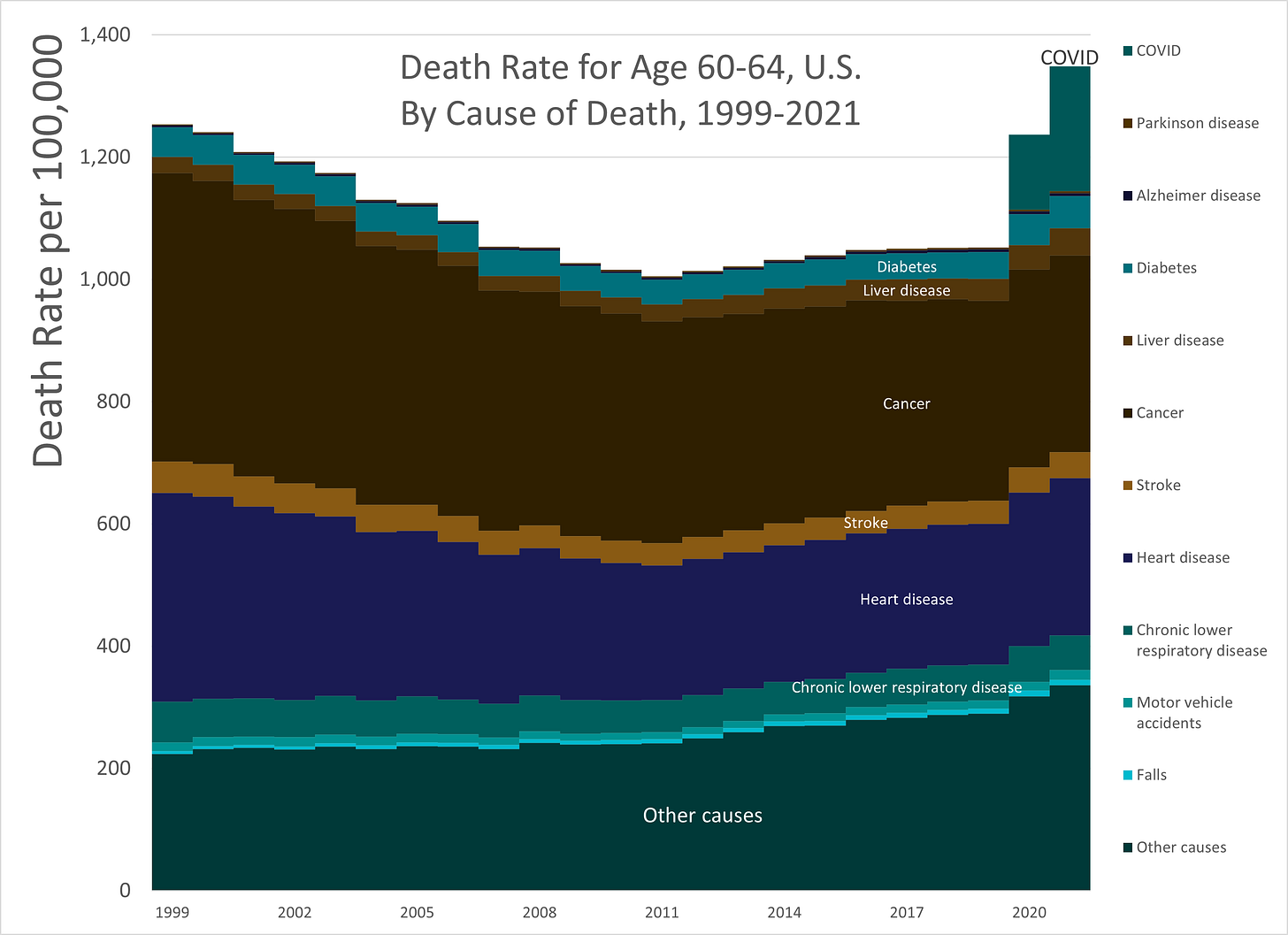
Longer trend, 1999-2021:
For all of these analyses, please pay close attention to the scale of rates. On this graph, the total mortality for 2021 is over 1,300 per 100,000. This is 1.3%. In 2019, it was about 1,000, or 1.0%.
When you hear people talking about a 1% chance of death, now you’ve got your age to attach it to — about age 60-64 for the death rate. That is about when total mortality is 1%.
As we step to higher ages, we will see this scale expand a lot, and we will see the areas for heart disease and cancer also expand a lot. These are the top two causes of death. I had these two in for younger age groups, but now I’ve put in more causes of death, as things have shifted with older people, and dropped others.
I dropped: drug overdoses, suicide, and homicide. Those are prominent causes of death for younger people, mainly because the “natural” death rates are fairly low. Suicide rates for older people are actually higher than for younger people, but the “natural” mortality level is so high, that suicide starts falling off the top ten causes of death.
I added in: falls, chronic lower respiratory disease, stroke, Alzheimer's disease, Parkinson's disease. These are more prominent at older ages. You can see where I labeled stroke and chronic lower respiratory disease on this graph, but can barely see the slivers for Alzheimer’s and Parkinson’s. Those slivers will get a bit bigger for older ages in absolute terms, but in relative terms, maybe not so much, as that vertical scale is going to become quite large quite rapidly.
Let’s focus just on the pandemic years.
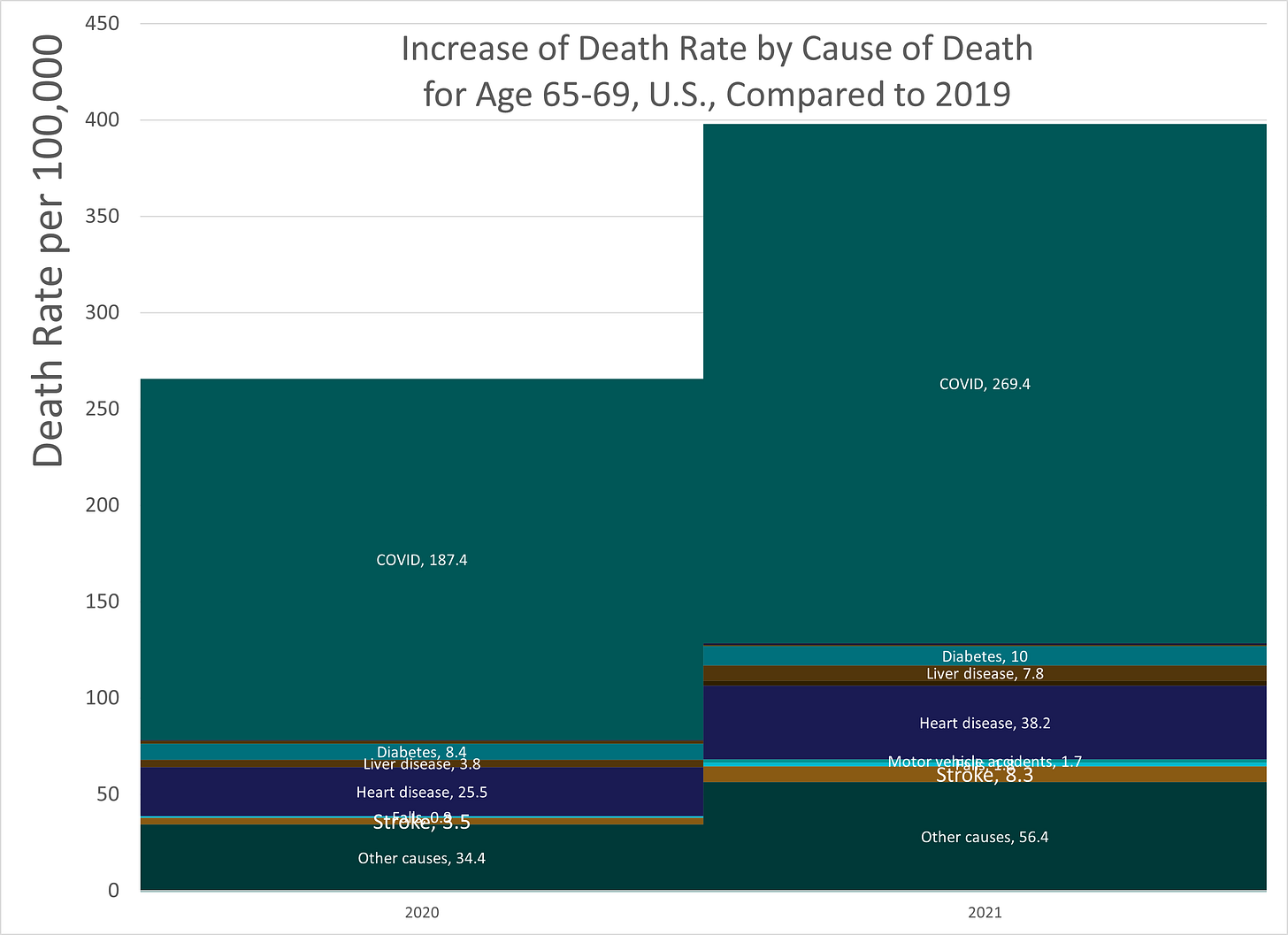
Attribution of increase in mortality, 2020-2021:
I will be doing this analysis for each age group. There will be a table at the end with the percentage breakout for each age group, but for now, let the contributions be the actual numbers and be the visual weight.
What you are seeing here are the rate increases (in per 100,000 per year amounts) by cause of death compared to 2019.
As mentioned in my key takeaways above, cancer and chronic lower respiratory disease actually provided (small) negative contributions, but I’m cutting off these graphs at zero, because I found them to be distracting.
Just look at that COVID.
LOOK AT IT.
Again, visually, we’re going to see that COVID contribution just drown out everything else.
You will see that “other causes” is fairly substantial. I did dig into it a bit, but I generally couldn’t find any particular causes that gave enough of a contribution compared to the others you see here. Heart disease was a clear contributor to increased mortality, as were liver disease and diabetes.
It may turn out a bunch of various causes increased due to lack of medical care in 2020 and 2021, which shows up more often in older adults than it does in younger adults (who die more often due to acute causes like car accidents and drug overdoses).
I picked the causes of death to investigate by the top ten by age group, and for accidental death sub-causes (like drug overdoses, motor vehicle accidents, and falls), I did my own categorization and ranking. This is what I got.
Age 65 – 69
Longer trend, 1999-2021:
I want to point out that there was a “flat” mortality period in the 2010s, where total mortality was going sideways.
If you dig down into the specific causes of death, there are several disturbing patterns and some good ones. Cancer was improving throughout, so that’s good. Heart disease actually got worse or went sideways starting around 2015. Liver disease also got worse starting around 2015. You can see that “other causes” also had been increasing.
Things weren’t all peaches and cream pre-pandemic, so that’s something to think about.
I will let you know two factoids:
1. Senior mortality in the U.S. improved once Medicare came into being, and seniors finally had guaranteed medical care financing (at least in hospitals). But that started way back in 1965.
2. Many U.S. men have increased mortality the year they retire from work. This doesn’t happen to women.
These may not be related to what happened starting in 2015, but it’s something to think about.
Attribution of increase in mortality, 2020-2021:
COVID is just going to keep growing in its visual percentage of this graph.
Age 70 – 74
Longer trend, 1999-2021:
This is a bit funky curve, in that it had its own mortality plateau, then kept improving. Something was going on in the 2010s. I wonder what.
Obamacare?
You can actually see the Parkinson’s and Alzheimer’s curves a little better, though I didn’t label them directly. They’re squeezed between diabetes and COVID. Alzheimer’s is actually growing in magnitude over time.
Note that the mortality level starts at about 3,000 in 1999 — that’s a 3% mortality rate.
Attribution of increase in mortality, 2020-2021:
The proportions are about the same as in the prior graph.
Age 75 – 79
Longer trend, 1999-2021:
Finally, the last group for this post.
This one doesn’t have that mortality plateau, but steady mortality improvement pre-pandemic. So that’s good there.
You can definitely see the significant Alzheimer’s contribution to mortality, and I tried to fit the label in. Yes, it is growing over time. This is one of the “bad” trends for older age.
Another bad trend is increasing mortality from falls (at the bottom of the graph), but its magnitude is far less than Alzheimer’s.
Attribution of increase in mortality, 2020-2021:
COVID makes a substantially larger contribution to the increase in mortality in proportion. It really dwarfs all the others.
Summary tables of contribution to excess mortality
For 2020
In the first column, I’m indicating how much mortality increased compared to 2019. So for the age 65-69 years group, their mortality increased 18% from 2019 to 2020, and of that increase, 73% is explained by COVID.
The amount mortality increased over this whole age range is fairly flat — from 17% to 18%. Not much of a difference. But note how different the mortality levels are — about 1.2% rate for age 60-64 and 4.0% for age 75-79. Think about how steep the mortality curve is over these 20 years. I will return to that at the end of the post.
The contribution COVID made to mortality increases is over two-thirds at all ages in the range, and heart disease made the next largest contribution of the top causes of death. You can see that cancer had gone down, as had chronic lower respiratory disease. The other major causes made small contributions.
But it’s mainly COVID.
For 2021
In 2021, the overall increase in mortality was higher — interestingly, it was least at the oldest ages, with only a 20% increase for those aged 75-79, and a 28% increase for the youngest age group in the range.
But again, COVID explains most of the increase. Heart disease contributed about the same amount of explanatory power, and the other major causes had their small contributions.
The main change of note was cancer — where it had been lower in 2020, we see that for ages 65-79, it had been a little higher in 2021. It’s not a large contribution, but for many who have been concerned that cancer patients may have been undertreated during the pandemic, perhaps this is some support.
Links to all the mortality posts
These will get updated as I fill in the posts
Young Adults — Age 18-39: approximately the Millennials in 2020-2021 Part 1 and Part 2, plus the podcast
Middle Agers — Age 40-59: approximately Gen X – Middle-aged Massacre (too!): Increase in Mortality for Ages 40-59 in the U.S. for 2020-2021 Mainly Driven By COVID
Young Seniors — Age 60-79: approximately Boomers – this post
Old Seniors — Age 80+: mainly Silent Generation (as older generations are mostly dead at this point) – to come
Age has an exponential effect on mortality
As noted in the Gen X post of mortality experience, age is the biggest driver of mortality differences, especially with respect to COVID.
I’ve written about a formula used in actuarial work called the Gompertz-Makeham function, which works for both mortality and morbidity, and works extremely well for certain types of “frailty” conditions. It generally works for physiological causes of death, total mortality rates, COVID death rates, and more.
In general, older people are frailer than younger people, and that frailty expresses itself in an exponential relationship. You can see in the tables above how rapidly the mortality rates of 2021 are climbing with each age group.
Many people do not like to think about these things, but it’s something to keep in mind. That the long-term trend has been to reduce those numbers has been a great achievement. Some of that achievement has been through lifestyle changes (fewer people smoking, primarily), and some through medical breakthroughs.
It’s sad that COVID wiped out, essentially, two decades’ worth of mortality improvement in those two years, but the hope is that COVID mortality is just passing. For the older ages, if COVID mortality goes away, the hope is that the mortality levels will return to fairly regular levels rapidly.
That said, we saw in the longer-term trends, some of the age groups were showing some concerning trends pre-pandemic. I’m not sure what was going on there.
Methodology
Data for deaths in 1999-2020 had been taken from the CDC WONDER Online Database for Underlying Cause of Death, finalized data. Citation: Centers for Disease Control and Prevention, National Center for Health Statistics. National Vital Statistics System, Mortality 1999-2020 on CDC WONDER Online Database, released in 2021. Data are from the Multiple Cause of Death Files, 1999-2020, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. Accessed at http://wonder.cdc.gov/ucd-icd10.html on August 3, 2022.
Data for deaths in 2021 had been taken from the CDC WONDER Online Database for provisional mortality data. Citation: Centers for Disease Control and Prevention, National Center for Health Statistics. National Vital Statistics System, Provisional Mortality on CDC WONDER Online Database. Data are from the final Multiple Cause of Death Files, 2018-2020, and from provisional data for years 2021-2022, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. Accessed at http://wonder.cdc.gov/mcd-icd10-provisional.html on August 14, 2022.
For cause of death, the ICD-10 113 Cause List had been used, and specific causes of death were used for their significance for these specific age groups. If this is on substack, you can download the accompanying spreadsheet to see the specific cause of death codes from the list of 113, and that they were non-overlapping. There was a catch-all “other causes” category used.
To measure the increase in mortality, a comparison against the year 2019 was used.
In all cases, crude death rates (based on population estimates provided in CDC WONDER) are used as provided by the CDC, using the standard rate per 100,000 people per year.
It is to be noted that some of the causes of death showed a decrease in rate in 2020 and 2021 compared to 2019 (most notably, cancer), though these were not large decreases.