October 2024: Breast Cancer Awareness Month and Advanced Breast Cancer
Improved treatment for metastatic breast cancer has large effect on improving breast cancer mortality
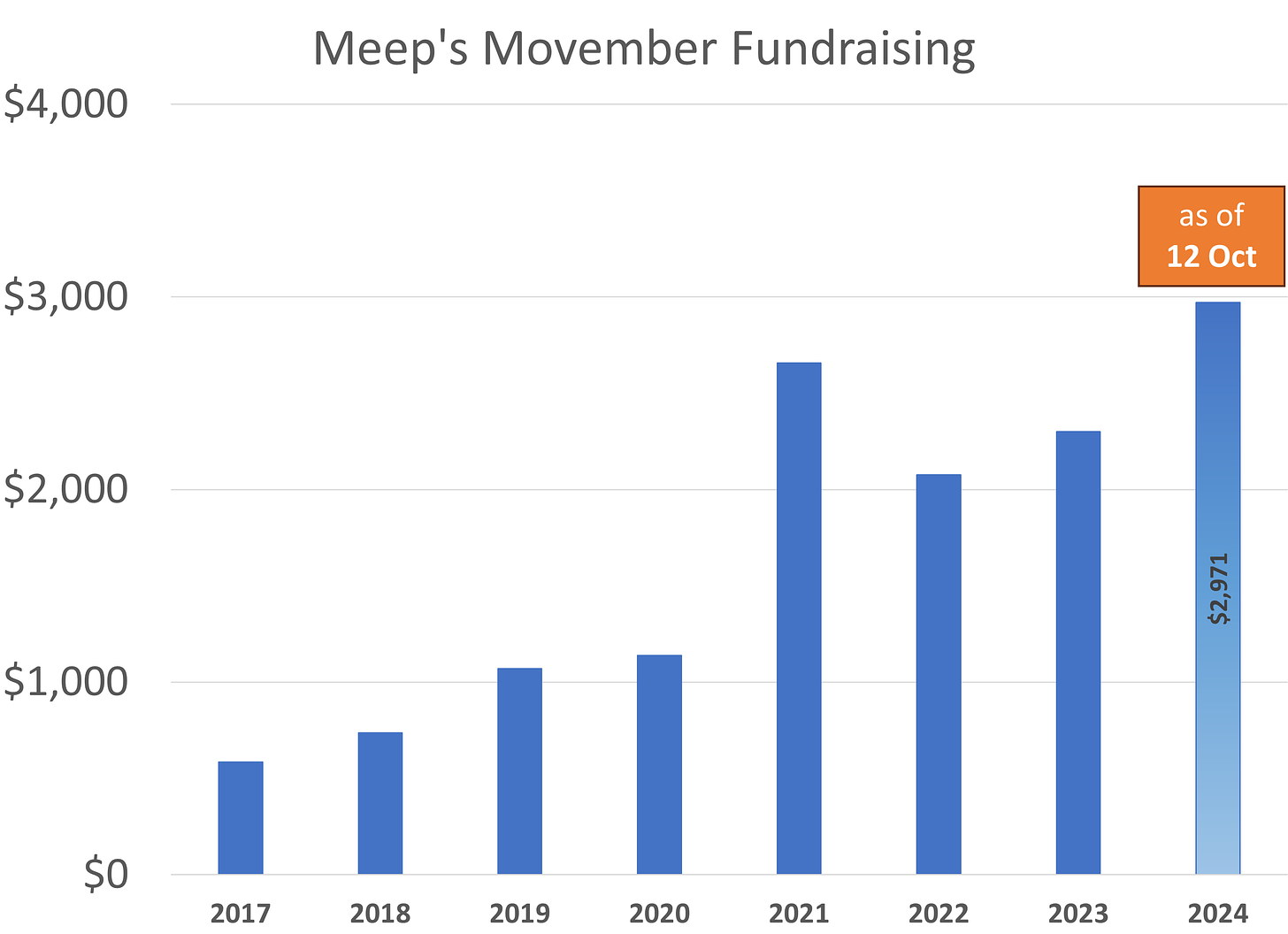
Before I get into the breast cancer statistics, thanks to everyone who has donated to Movember in memory of my late husband Stuart, who had died from complications related to advanced prostate cancer:
I will be doing my normal Movember fundraising when November rolls around, and I will be talking more about it then. Many of y’all have donated to my fundraisers in past years, and I really appreciate the support.
October: Breast Cancer Awareness Month
It isn’t a competition between breast cancer and prostate cancer. There is a linkage between treating these cancers, especially the advanced types. The oncologists Stuart saw treated both advanced breast and prostate cancer, especially the hormone-sensitive types. I will be talking about that a little more below.
October is Breast Cancer Awareness Month, which was started in 1985 as a campaign between the American Cancer Society and Imperial Chemical Industries.
You may be scratching your head over that second group’s name, but they manufactured tamoxifen, a breast cancer treatment. Specifically, tamoxifen is used in treating advanced estrogen receptor-positive breast cancer.
Here is a paper on the history of tamoxifen: Tamoxifen from Failed Contraceptive Pill to Best-Selling Breast Cancer Medicine: A Case-Study in Pharmaceutical Innovation
That gives you an idea of some of what was going on there, and if you read the paper, you will see that hormone-sensitive prostate cancer shows up in this history. I noticed that in Stuart’s treatments.
But remember the year 1985, because let us look at breast cancer mortality trajectory in the U.S. at a high level.
Age-adjusted Death Rate of Breast Cancer in U.S., Females, 1968-2023
While males do also suffer from breast cancer and can die from it, let me simplify by focusing on breast cancer among females in the U.S. It is a top deadly cancer for females, other than lung cancer and colorectal cancer.
(Ignore the 2021 “burp” in the graph above - it’s spurious.)
Before 1988, there had been no improvement in breast cancer mortality in the U.S. But since 1988, there has been a cumulative 43% decrease in age-adjusted death rates among females in America overall. That is equivalent to a 1.6% per year compounded improvement over the 35-year period.
The improvement in breast cancer outcomes since about 1990, especially in mortality, had been noted in the academic literature, and trying to determine whether screening, treatment, and what types of treatment had the most effects has been a topic of discussion since the mid-1990s.
On Advanced Breast Cancer
Back in July, I posted about the death of Shannen Doherty:
She had originally been diagnosed with breast cancer in 2015, which had been in remission by 2017, but came back as an advanced case in 2020. By 2023 the cancer had spread to her bones and brain, and she had brain surgery. She died in July 2024.
Advanced cancer, or metastatic cancer, where the cancer has spread beyond the original site, is difficult to deal with, and the treatments can be quite harsh.
Many breast cancer survivors have their cancer detected and never see metastatic or advanced breast cancer. However, the survival rates for this diagnosis, should the cancer spread beyond the original site, are not high.
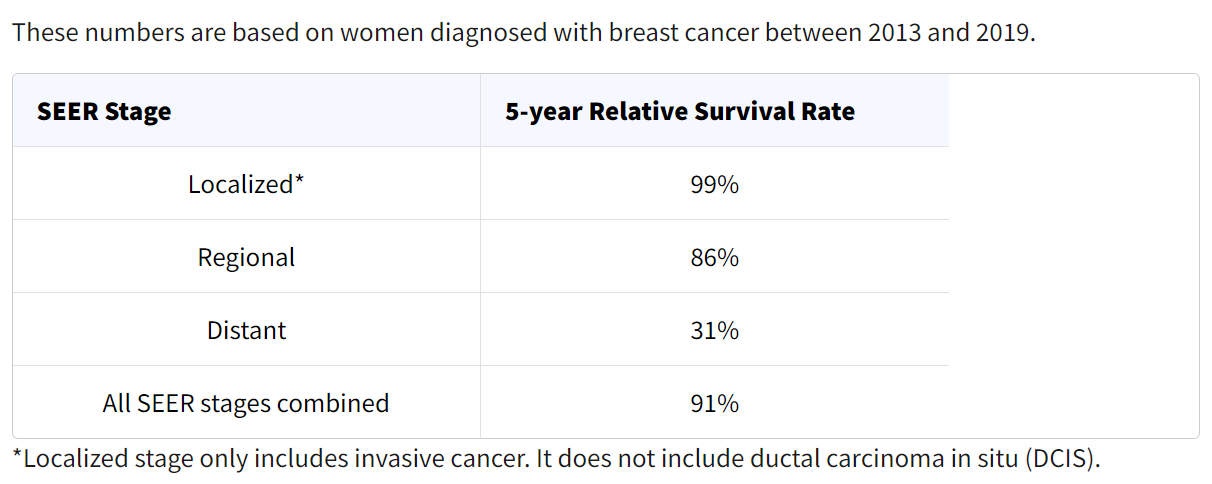
Breast Cancer Survival Rates by Stage
The current best estimate of survival rates, from the American Cancer Society:
“Distant” is where the cancer cells are distant from where they originated, which is often called advanced breast cancer. A 31% survival rate is not high.
That said, it is a lot higher than it used to be.
Treatment of Advanced Breast Cancer Has Had a Large Effect on Breast Cancer Mortality in U.S.
From January 2024, Stanford University press release: Metastatic breast cancer treatments have aided decline in deaths, Stanford Medicine-led study finds
Deaths from breast cancer dropped 58% between 1975 and 2019 due to a combination of screening mammography and improvements in treatment, according to a new multicenter study led by Stanford Medicine clinicians and biomedical data scientists.
Nearly one-third of the decrease (29%) is due to advances in treating metastatic breast cancer —a form that has spread to other areas of in the body and is known as stage 4 breast cancer or recurrent cancer. Although these advanced cancers are not considered curable, women with metastatic disease are living longer than ever.
The analysis helps cancer researchers assess where to focus future efforts and resources.
….
The impact of treating metastatic disease is exemplified by the increases in median survival time after metastasis: Patients diagnosed in 2000 with metastatic disease lived an average of 1.9 years versus an average of 3.2 years for those diagnosed in 2019. Survival time varies by subgroup status, however. Patients with what are known as estrogen receptor-positive and HER2 positive cancers saw an average increase in survival time of 2.5 years. Those with estrogen receptor-positive and HER2-negative cancers lived an average of 1.6 years longer, but those with cancers that are estrogen receptor-negative and HER2-negative lived about 0.5 years longer in 2019 than in 2000.
It gets quite complicated, because all of these effects depend on the incidence of the different types of cancers in the population.
Most of the breast cancer diagnosed in the population is localized, not distant (metastatic). Most of the localized cancer will not metastasize. Of the cancers that metastasize, you get a certain proportion that are estrogen-receptor positive, etc.
That said, of those who die of breast cancer, most will be due to metastasis. So one can understand why improved treatment of advanced breast cancer had such a large effect on breast cancer mortality overall.
Let us go to the academic paper to look at the effects. I went to the first-named author on the paper’s publication page: Jennifer Caswell-Jin Publications
Analysis of Breast Cancer Mortality in the US-1975 to 2019. JAMACaswell-Jin, J. L., Sun, L. P., Munoz, D., Lu, Y., Li, Y., Huang, H., Hampton, J. M., Song, J., Jayasekera, J., Schechter, C., Alagoz, O., Stout, N. K., Trentham-Dietz, A., Lee, S. J., Huang, X., Mandelblatt, J. S., Berry, D. A., Kurian, A. W., Plevritis, S. K.2024; 331 (3): 233-241
Abstract
Breast cancer mortality in the US declined between 1975 and 2019. The association of changes in metastatic breast cancer treatment with improved breast cancer mortality is unclear.To simulate the relative associations of breast cancer screening, treatment of stage I to III breast cancer, and treatment of metastatic breast cancer with improved breast cancer mortality.Using aggregated observational and clinical trial data on the dissemination and effects of screening and treatment, 4 Cancer Intervention and Surveillance Modeling Network (CISNET) models simulated US breast cancer mortality rates. Death due to breast cancer, overall and by estrogen receptor and ERBB2 (formerly HER2) status, among women aged 30 to 79 years in the US from 1975 to 2019 was simulated.Screening mammography, treatment of stage I to III breast cancer, and treatment of metastatic breast cancer.Model-estimated age-adjusted breast cancer mortality rate associated with screening, stage I to III treatment, and metastatic treatment relative to the absence of these exposures was assessed, as was model-estimated median survival after breast cancer metastatic recurrence.The breast cancer mortality rate in the US (age adjusted) was 48/100 000 women in 1975 and 27/100 000 women in 2019. In 2019, the combination of screening, stage I to III treatment, and metastatic treatment was associated with a 58% reduction (model range, 55%-61%) in breast cancer mortality. Of this reduction, 29% (model range, 19%-33%) was associated with treatment of metastatic breast cancer, 47% (model range, 35%-60%) with treatment of stage I to III breast cancer, and 25% (model range, 21%-33%) with mammography screening. Based on simulations, the greatest change in survival after metastatic recurrence occurred between 2000 and 2019, from 1.9 years (model range, 1.0-2.7 years) to 3.2 years (model range, 2.0-4.9 years). Median survival for estrogen receptor (ER)-positive/ERBB2-positive breast cancer improved by 2.5 years (model range, 2.0-3.4 years), whereas median survival for ER-/ERBB2- breast cancer improved by 0.5 years (model range, 0.3-0.8 years).According to 4 simulation models, breast cancer screening and treatment in 2019 were associated with a 58% reduction in US breast cancer mortality compared with interventions in 1975. Simulations suggested that treatment for stage I to III breast cancer was associated with approximately 47% of the mortality reduction, whereas treatment for metastatic breast cancer was associated with 29% of the reduction and screening with 25% of the reduction.
As mentioned in the abstract, the estimated effects came from modeling, and ranges are given for the potential effects. Here is the structure of their model for timeline:
To be sure, for some aggressive cancers, the cancer is not found until after the cancer has metastasized (this was the case with Stuart and his cancer.)
They mention the limitations of their model:
This study has several limitations. First, the model accuracy depends on the assumptions made, for which accurate data were not always available. Second, the models did not incorporate potential disparities, for example, by age, race, and ethnicity, in dissemination or efficacy of screening and treatments. Disparities in breast cancer screening, as well as timeliness and quality of treatment, may contribute to differential breast cancer mortality rates.23 Third, treatment costs and their associations with outcomes were not included in the models.
They are parameterizing their model based on the best data they have. Much of the model risk/uncertainty can be seen in the ranges in the results.
However, for metastatic survival, an increase from an average 1.9 years survivorship to 3.2 years (an increase of 1.3 years) is huge from a percentage standpoint.
Having just lived through the equivalent for prostate cancer, where Stuart survived 7 years with an initial metastatic cancer diagnosis, I can attest the increase in lifetime with the drugs for hormone-sensitive cancers has been fabulous. The 7 years were far longer than the expected lifetime used to be. We’re seeing this for both prostate and breast cancer and it is showing up in the broader population statistics. They don’t tell you expected lifetime now, not only because it’s too depressing, but because the treatments have been developing so rapidly.
So: a little less than half of the reduction is coming from treatment for early stages of breast cancer. About a fourth is coming from breast cancer screening.
Almost 30% of the mortality improvement has come from improved treatment of advanced breast cancer.
While screening is not necessarily changing much, the treatments continue to be developed. I am optimistic that advanced cancer treatments will continue to improve.






Thank you for taking the time with all that is going on to keep up with great work like the breast cancer survival update. My sympathies to you and your family.
Back more than a few years I read an article on some breast cancer doctors in Boston who feared the arrival of October – what they called “Pinktober” because of how hard the news reports and events were on advanced cancer patients. It was a time that the same thing had really bugged me. “Save the Boobs” t-shirts sold in bars. Chicago Bears game attendees given pink postcards with mammography information to take home to their wives. Is that an effective tool?
Although my wife did well decades ago with treatment of a localized case, I didn’t want to bring home routine prescription drugs for me or her with pink lids instead of white. You should have heard my discussion with the pharm-tech at the drug store. Me: you mean you don’t have any white lids in the store. Are you getting a special delivery of them on November 1st? Her: it's for breast cancer.
Anyway, it has really calmed down over the years. Thanks for the info.
Dan, Skokie IL