Update on Michelle Trachtenberg Death: Plus U.S. Diabetes Mortality Trends 1999-2024
Yes, the title gives it away, but there may be some confusions...
This may explain some things. This is a follow-up to my earlier post: RIP, Michele Trachtenberg: Some Stats on Liver Disease Mortality.
Earlier, in the immediate shock of her death, some had been assuming her death was related to a recent liver transplant. But this was rumored information.
People Magazine, 16 April 2025: Michelle Trachtenberg's Official Cause of Death Revealed After Gossip Girl Star Died at 39
Michelle Trachtenberg's cause of death has been revealed.
The New York City Office of Chief Medical Examiner confirmed to PEOPLE on Wednesday, April 16, that the actress' sudden death was a result of complications of diabetes mellitus. The manner of death was ruled as natural.
This comes less than two months after Trachtenberg was found dead in a New York City apartment when law enforcement responded to a 911 call on Feb. 26. After officers arrived, they found a woman, identified as Trachtenberg, unconscious and unresponsive.
The New York City Medical Examiner's Office told PEOPLE the next day that the Gossip Girl alum's family objected to an autopsy, meaning that her cause of death would be ruled "undetermined."
That last bit is not true, by the way. [as it turned out, according to the reporting from PEOPLE.]
Autopsies are not required to determine the cause of death
There are levels of examination where one can determine the cause of death without a full autopsy.
I am not getting into the details, but here is an example FAQ from Cook County, Illinois:
What is an autopsy?
An autopsy is a thorough examination of the body, inside and out, performed to document or rule out injuries and diseases. The procedure is performed by a medical doctor with special forensic training in recognizing the appearance of injuries and the effects of diseases. An autopsy may take 2-3 hours or longer to perform and is often followed by laboratory tests, some of which can take months to complete.
Will an autopsy always be performed?
No. An autopsy is performed at the medical examiner’s discretion based on all of the information available at the time of examination. An autopsy may not be required when the death is known to be the result of natural causes, adequate medical history exists, and there are no signs of foul play. Autopsies are required when there is evidence or reasonable suspicion of foul play.
There is additional detail after that, going into the details for suspicion of suicide, homicide, or accidental death.
An autopsy involves dissection of the body, but the medical examiner can do less invasive tests, such as toxicology screens on the blood.
I assume they found signs of diabetic coma from such a screen.
Uncontrolled Diabetes Can Lead to Rapid Weight Loss
People have commented on Trachtenberg’s appearance, and many opined on potential drug abuse, GLP-1 use, eating disorders, and all sorts of things.
It may have been uncontrolled diabetes.
One symptom of undiagnosed Type 1 diabetes is unexplained weight loss.
The picture I had used in my prior post, I will use again: Trachtenberg in 2018.

The PEOPLE article has pictures from 2019 and 2020, and she still looked similar to the above. No noticeably shocking thinness.
But in January of this year:
And Feb 12:
That last one may have some camera effects/filters going on, and it’s difficult to gauge simply looking at cheeks and chin, because that’s basically all we have to go on.
So here’s the deal: organ transplants can spur diabetes.
Post-Transplant Diabetes Mellitus: Causes, Treatment, and Impact on Outcomes
by Vijay Shivaswamy, Brian Boerner, Jennifer Larsen
Endocrine Reviews, Volume 37, Issue 1, 1 February 2016, Pages 37–61, https://doi.org/10.1210/er.2015-1084
Abstract:
[emphasis added]
Post-transplant diabetes mellitus (PTDM) is a frequent consequence of solid organ transplantation. PTDM has been associated with greater mortality and increased infections in different transplant groups using different diagnostic criteria. An international consensus panel recommended a consistent set of guidelines in 2003 based on American Diabetes Association glucose criteria but did not exclude the immediate post-transplant hospitalization when many patients receive large doses of corticosteroids. Greater glucose monitoring during all hospitalizations has revealed significant glucose intolerance in the majority of recipients immediately after transplant. As a result, the international consensus panel reviewed its earlier guidelines and recommended delaying screening and diagnosis of PTDM until the recipient is on stable doses of immunosuppression after discharge from initial transplant hospitalization. The group cautioned that whereas hemoglobin A1C has been adopted as a diagnostic criterion by many, it is not reliable as the sole diabetes screening method during the first year after transplant. Risk factors for PTDM include many of the immunosuppressant medications themselves as well as those for type 2 diabetes. The provider managing diabetes and associated dyslipidemia and hypertension after transplant must be careful of the greater risk for drug-drug interactions and infections with immunosuppressant medications. Treatment goals and therapies must consider the greater risk for fluctuating and reduced kidney function, which can cause hypoglycemia. Research is actively focused on strategies to prevent PTDM, but until strategies are found, it is imperative that immunosuppression regimens are chosen based on their evidence to prolong graft survival, not to avoid PTDM.
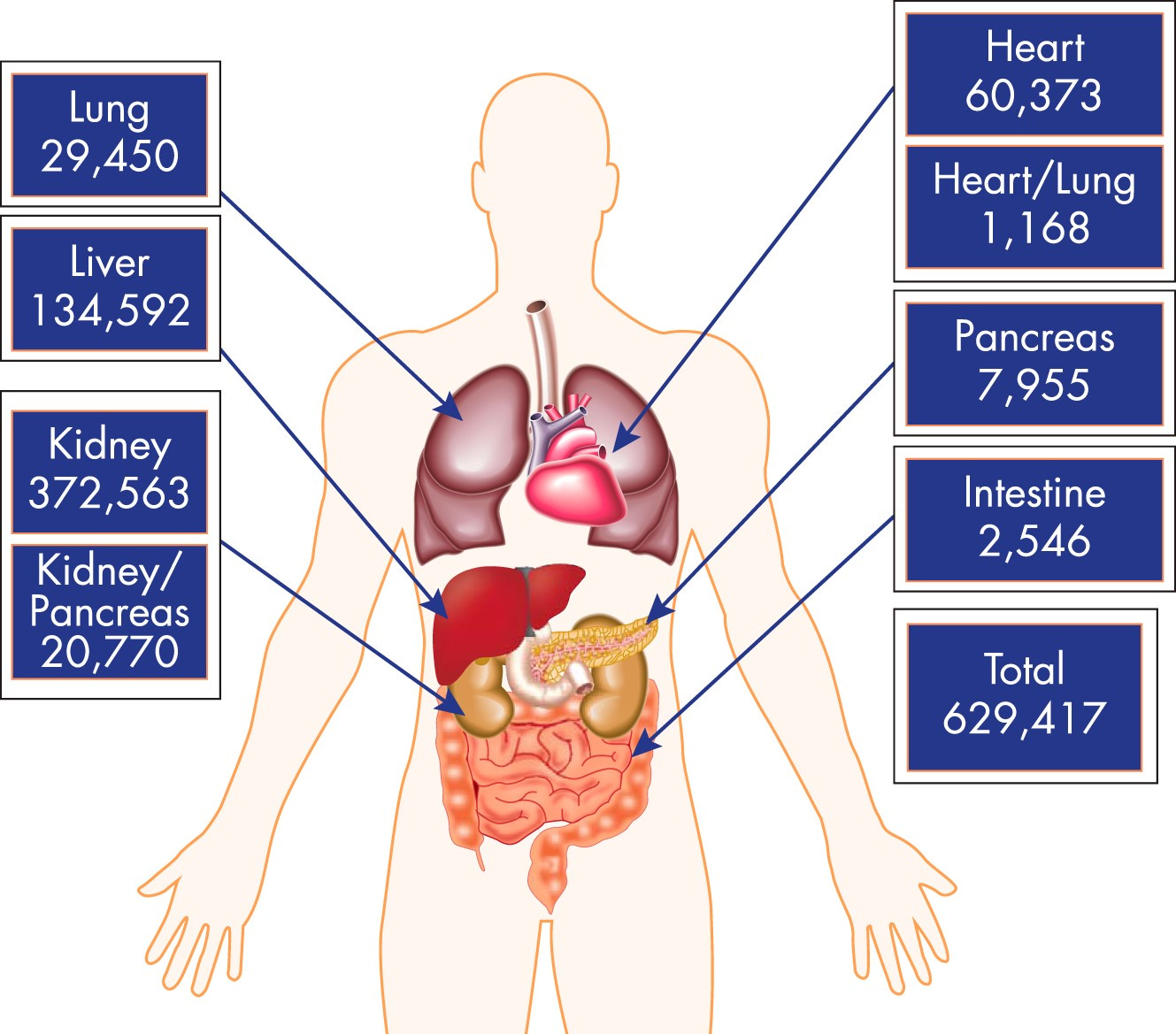
My Aunt Pat had a kidney/pancreas transplant in an attempt to cure her Type 1 diabetes. Alas, she ultimately died. Organ transplantation is difficult.
Note that kidney and liver transplants are most common, which is not surprising, since those can be donated by live donors. You need only one kidney, and you can donate parts of your liver. It is much easier to complete transplants when you don’t have to wait around for someone to die in perfect condition.
Pulling back to Michelle Trachtenberg’s case, diabetes may have directly been the cause of death, but her liver transplant may have caused diabetes that led to her death.
Let me go to recent trends on death due to diabetes in the U.S. — we’ll see some odd results.
Diabetes Death Trends in the U.S. — 1999-2024
The 2024 data I have are provisional, so keep that in mind.
While the 2024 data are provisional, the other years are finalized. (There are issues with 2021, but I don’t want to get into that right now. Hey, CDC, can y’all redo that data? Thanks!)
I will talk a little more about the pandemic trend in a section below, so let us focus on the pre-pandemic trend.
The age-adjusted death rate improved notably from 2004 to 2009, then stalled.
That’s the story.
If we break it out by age group, you can see the steadier improvement for the oldest age group, and the stagnation (or disimprovement) at younger age groups.
It’s difficult to see in the graph, given the scale difference. Unsurprisingly, for this natural cause of death, the oldest age group has a death rate that is at a magnitude much higher than the younger groups.
When we look at the age groups split out, then we see the younger ages disimproving (though we’ll see below there may be pandemic effects), and decent improvements for the older age groups.
One problem is that it’s all one category of “diabetes” — Type 1 and Type 2 are of different natures, and death due to diabetes at young ages have tended to be related to Type 1 diabetes, which is an autoimmune disease. Type 2 diabetes is more a metabolic disease.
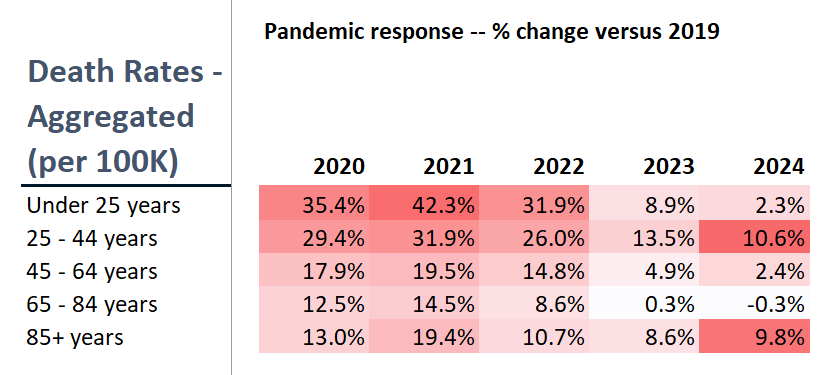
Diabetes Deaths: Focus on the Pandemic Response
That was the long-term change — let’s look at just what happened during the pandemic, because there was quite a bobble.
Again, the differences in magnitude make it difficult to see the movements at younger ages.
In the final column, I’m comparing 2024 provisional stats against 2019. You can see that in many cases, 2023 was higher than 2024 (provisionally).
2020 and 2021 were higher than that.
Yeaaaaah.
Some of this is a matter of sensitivity to a small number of deaths — not many people die from diabetes under the age of 45.
Usually.
But something about the Age of COVID changed that. And the ages 25-44 years is showing persistently high rates compared to pre-pandemic rates.
This is not good.