I said I’d take a deeper dive into mortality trends in the U.S., up to the final data from 2017.
There are some mortality stats from 2020, and I will look at that in my next mortality-related post.
First, in video form:
Below, I’m pulling some of the major figures from the final death data of 2017 study.
Difference between Crude and Age-Adjusted Death Rates
Figure 1 from the study:
The crude death rate, or what I also called the raw mortality rate, of just under 1% has been around that level for decades. In the above figure, you see that there was a drop in the crude death rates somewhere in the mid-1970s, as the baby boomer bulge started working through the population, as well as great improvement in mortality at older ages.
One day I will visualize mortality improvement by age ranges… but today is not that day. In the 20th century, most of the improvement originally came from reduction in death by infectious disease, at the end of the century, it was mainly improvement in heart disease-related mortality as there had been a great drop in smoking rates and a widespread use of effective drugs, and lately improvements are primarily related to cancer. We will come to that in a bit.
My point is that if you just looked to the crude death rate, there would not seem to be much of an improvement for over 50 years.
That is why looking at the age-adjusted death rate is useful. It tries to capture in one number how mortality levels have improved across all ages.
The following is from table 1, on page 22 — it’s not in the above graph. The age-adjusted death rate in 1940 was about 1.8%. [The crude rate then was 1.4%]
In 1960, the age-adjusted death rate was 1.3%, and was still above 1.0% in 1980.
In 2017, that age-adjusted death rate was 0.7%. The age-adjusted death rate has more than halved since 1940, and about halved since 1960. That’s fabulous. The steepest drop was between 1970 and 1980…. unfortunately, the age-adjusted death rate has increased a little since 2014. It’s kind of sideways, though.
Age-adjusted Death Rates by Ethnicity
Figure 2 of the study:
There will be a few related figures on this subject, but I want to point out: these are age-adjusted death rates.
The difference here has nothing to do with non-Hispanic white populations being, in general, an older skewed population compared to other ethnic groups.
The difference that surprises nobody is the white-black mortality gap [though, as will become more clear, that gap has been narrowing].
The difference most people are unaware of: the Hispanic-White gap. However, that may be partly due to misclassification. There is this note in the study:
Mortality for Hispanic persons may be somewhat
understated because of net underreporting of Hispanic origin on
the death certificate (by an estimated 3%), while data for the
non-Hispanic white and non-Hispanic black populations are not
affected by problems of underreporting (20,21); see Technical
Notes.
If you jump to the Technical Notes, you get this:
Quality of race and Hispanic-origin data—Death rates for
Hispanic, non-Hispanic AIAN, and non-Hispanic API persons
should be interpreted with caution because of inconsistencies
in reporting Hispanic origin or race on the death certificate
compared with censuses, surveys, and birth certificates. Studies
have shown underreporting on death certificates of non-Hispanic
AIAN, non-Hispanic API, and Hispanic decedents, as well as
undercounts of these groups in censuses (20,21,58,59).
A number of studies have been conducted on the reliability
of race and Hispanic origin reported on the death certificate by
comparing it with race and Hispanic origin reported on another
data collection instrument, such as the census or a survey
(20,21,60,61). Inconsistencies may arise because of differences
in who provides race and ethnicity information on the compared
records. Race and Hispanic-origin information on the death
certificate is reported by a funeral director as provided by an
informant or, in the absence of an informant, on the basis of
observation. In contrast, race and Hispanic origin in the census
or the U.S. Census Bureau’s American Community Survey (ACS)
is obtained while the person is alive; in these cases, race and
ethnicity is self-reported or reported by another member of
the household familiar with the person and, therefore, may be
considered more valid. A high level of agreement between the
death certificate and the census or survey report is essential to
ensure unbiased death rates by race and ethnicity.
In short, the official difference in mortality rates seen here may be due to under-reporting of Hispanic status in death. Basically, people who identified as Hispanic when alive may not have been when dead, as the funeral director may assume status based on last name. Plenty of Hispanic people do not have Spain- or Portugal-derived last names.
Luckily, it sounded like the disparity was about 3%.
Death Rates by Age and Sex
Figure 3:
This is a figure I need to address in greater detail in a future post.
In particular: when did mortality improve for each age group, and by how much? [Or, when did mortality “disimprove”?]
Most of the news is good. If you want to know about the bad news, take an eyeball for the 25-34 age groups. Look at what happens at the end of the curve. That is not good news.
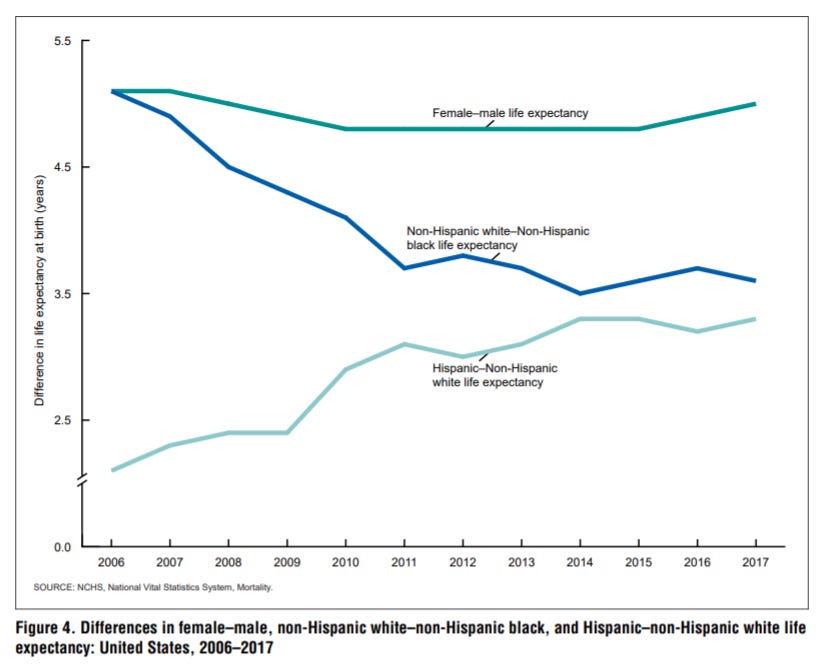
Life Expectancy Gaps by Sex and Ethnicity
Figure 4:
Let us ignore the Hispanic-NHW gap. It could be that the reporting gap may be driving that gap, but who knows.
But here is something to think about:
The sex gap in mortality is very high and persistent [though that is over a relatively short period of 11 years]
Even in 11 years, there was a decrease in the white-black mortality gap of about 1 year in life expectancy. That’s pretty good.
The sex gap in mortality is something that comes up again and again. While I do like to point to the stupidity period, that is not something that holds in all countries… though the sex gap in mortality does appear in pretty much every country. It’s not just smoking rates, doing-stupid-stuff rates, having riskier jobs, etc. Men seem to be more genetically fragile – one thing that punches one in the face re: COVID-19 is the sex gap in mortality. It’s even more stark than the usual mortality difference.
Here is Figure 5:
This projects the male/female, NH-white/NH-black/Hispanic life expectancy combos, and you can see how the gaps interact. Because the sex gap is far bigger than the ethnicity gaps, black women tend to live longer than white men. It’s something people generally don’t think about.
Age-Adjusted Death Rates by Cause of Death
Figure 6, the last one I’ll cover:
This is another figure that requires multiple posts to cover.
What I want to point out: great improvement with death rate for heart disease… and that cancer is pretty much level.
Another thing to point out: the increase in mortality due to Alzheimer’s & Parkinson’s diseases. Part of that is due to improvement in diagnosis, but in recent decades, the increase is real. I will talk about this later when I look at recent research from the Society of Actuaries. We are so used to most causes of death showing decreasing mortality trends over history, that we immediately notice when any of them have an increasing trend.
Happy Easter!
If you’d like a less statistical, and a more religious [or simply more musical] treatment of death, have my favorite Easter-related composition.
Bach’s St. Matthew Passion:
Happy Easter!
Original STUMP post: Mortality with Meep: Major U.S. Mortality trends 1955-2017