Covid Round-Up: Nursing Homes, Mortality Rates, Herd Immunity, and More
Also, I continue to complain about how bad the data are
The Actuarial Outpost seems really most sincerely dead, so I’m continuing my news round-ups on my favorite themes. Today’s theme is COVID.
Nursing home deaths in New York
I had some of this post in draft for over two months. Every time I think about this, I get angry, and you shouldn’t blog angry. Well, I shouldn’t blog angry.
Anyway, my hook today is someone in mainstream news FINALLY calling Gov. Cuomo out on COVID & nursing homes.
CNN: Fact check: Gov. Cuomo falsely claims New York nursing homes never took in Covid-positive patients
New York Gov. Andrew Cuomo argued that nursing homes “never needed” to accept Covid-positive patients from hospitals in the state.
During a press call Wednesday, Finger Lakes News Radio asked Cuomo about his administration’s advisory in late March requiring that nursing homes accept the readmission of patients from hospitals, even if they were positive for Covid-19.
Cuomo argued that the advisory was a precaution if hospitals became overwhelmed — calling it an “anticipatory rule” — which he said didn’t happen.
This is such an incredibly stupid lie. There are other ways he could’ve covered the problem: that COVID was widespread, and we didn’t know how bad it was, yadda yadda.
Don’t tell a lie about something that is very well documented.
Facts First: Cuomo’s assertion that “it never happened” is false. According to a report from the New York State Department of Health, “6,326 COVID-positive residents were admitted to [nursing home] facilities” following Cuomo’s mandate that nursing homes accept the readmission of Covid-positive patients from hospitals. Whether or not this was “needed,” it did in fact happen.
On March 25, the state’s Health Department issued an advisory requiring nursing homes to accept “the expedited receipt of residents returning from hospitals” if the patients were deemed medically stable.
“No resident shall be denied re-admission or admission to the [nursing home] solely based on a confirmed or suspected diagnosis of COVID-19,” the advisory stated. “[Nursing homes] are prohibited from requiring a hospitalized resident who is determined medically stable to be tested for COVID-19 prior to admission or readmission.”
It links to two documents: Factors Associated with Nursing Home Infections and Fatalities in New York State During the COVID-19 Global Health Crisis dated July 20, 2020 and Advisory: Hospital Discharges and Admissions to Nursing Homes dated March 25, 2020.
If it was a situation of “we said IF” instead of the real “we’re telling you to do this” order, then why did this next step occur:
This mandate received a great deal of criticism, and Cuomo issued an executive order changing the advisory on May 10 by requiring hospitals to be sure patients tested negative before discharging them to nursing homes.
By May 10, the New York COVID mortality spike was way down. The dead nursing home residents were already dead.
At the end of August, the Dept. of Justice issued this press release: Department of Justice Requesting Data From Governors of States that Issued COVID-19 Orders that May Have Resulted in Deaths of Elderly Nursing Home Residents
I’ll just quote it:
Today the Justice Department requested COVID-19 data from the governors of states that issued orders which may have resulted in the deaths of thousands of elderly nursing home residents. New York, New Jersey, Pennsylvania, and Michigan required nursing homes to admit COVID-19 patients to their vulnerable populations, often without adequate testing.
For example, on March 25, 2020, New York ordered: “No resident shall be denied re-admission or admission to [a nursing home] solely based on a confirmed or suspected diagnosis of COVID-19. [Nursing homes] are prohibited from requiring a hospitalized resident who is determined medically stable to be tested for COVID-19 prior to admission or readmission.”
…..
The Department of Justice’s Civil Rights Division is evaluating whether to initiate investigations under the federal “Civil Rights of Institutionalized Persons Act” (CRIPA), which protects the civil rights of persons in state-run nursing homes, among others. The Civil Rights Division seeks to determine if the state orders requiring admission of COVID-19 patients to nursing homes is responsible for the deaths of nursing home residents.
It’s a stupid lie. And it’s just the start of lies with NY nursing home deaths.
The problem with nursing home COVID mortality is that New York is hiding its stats. They’ve been counting nursing home/assisted-care homes COVID deaths as hospital deaths if the resident managed to get to the hospital and died there. Obviously, most of the nursing home COVID cases end up at the hospital, if it’s really that bad.
New York’s true nursing home death toll cloaked in secrecy
Riverdale Nursing Home in the Bronx appears, on paper, to have escaped the worst of the coronavirus pandemic, with an official state count of just four deaths in its 146-bed facility.
The truth, according to the home, is far worse: 21 dead, most transported to hospitals before they succumbed.
……
New York’s coronavirus death toll in nursing homes, already among the highest in the nation, could actually be a significant undercount. Unlike every other state with major outbreaks, New York only counts residents who died on nursing home property and not those who were transported to hospitals and died there.That statistic could add thousands to the state’s official care home death toll of just over 6,600. But so far the administration of Democratic Gov. Andrew Cuomo has refused to divulge the number, leading to speculation the state is manipulating the figures to make it appear it is doing better than other states and to make a tragic situation less dire.
I have no reason to trust Cuomo on this matter.
Back in May, FREOPP found that nationwide, over 40% of COVID deaths were nursing home-related. If you look at their map, they have NY COVID deaths as being 15% nursing home related. There is no way that is close to true.
Okay, I’m starting to get angry again, so onto a happier subject: death rates.
How to think about COVID mortality?
Wirepoints: New CDC Estimates: Fatality Rate For COVID-19 Drops Again And May Surprise You – Wirepoints
1 out of 34,000 for ages 0 to 19;
1 out of 5,000 for ages 20 to 49;
1 out of 200 for ages 50 to 69; and
1 out of 20 for ages 70 and up.
These are the current approximate infection fatality rates, meaning the likelihood you will die if you’re infected with COVID.
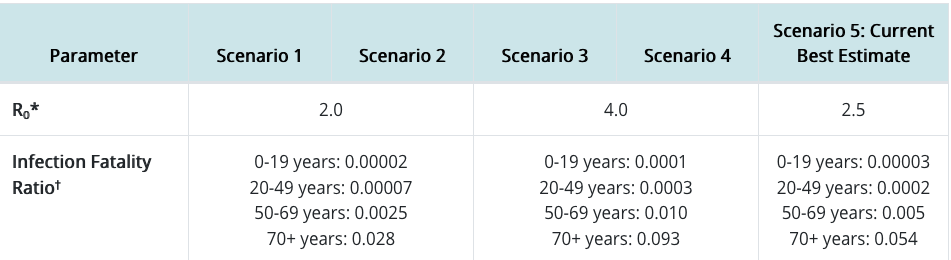
Here are the actual numbers from the CDC:
So here’s the deal: do you know how meaningful those amounts are?
Here’s another way to look at those probabilities:
Age Group Probability of Survival
0-19: 99.9997%
20-49: 99.98%
50-69: 99.5%
70+: 94.6%
Okay, but do you know what your annual survival rate is without COVID?
A 5% death rate, the estimated IFR for those age 70+, is actually very high. The age at which the q_x (one-year death rate at age x) is 5% is about age 81.
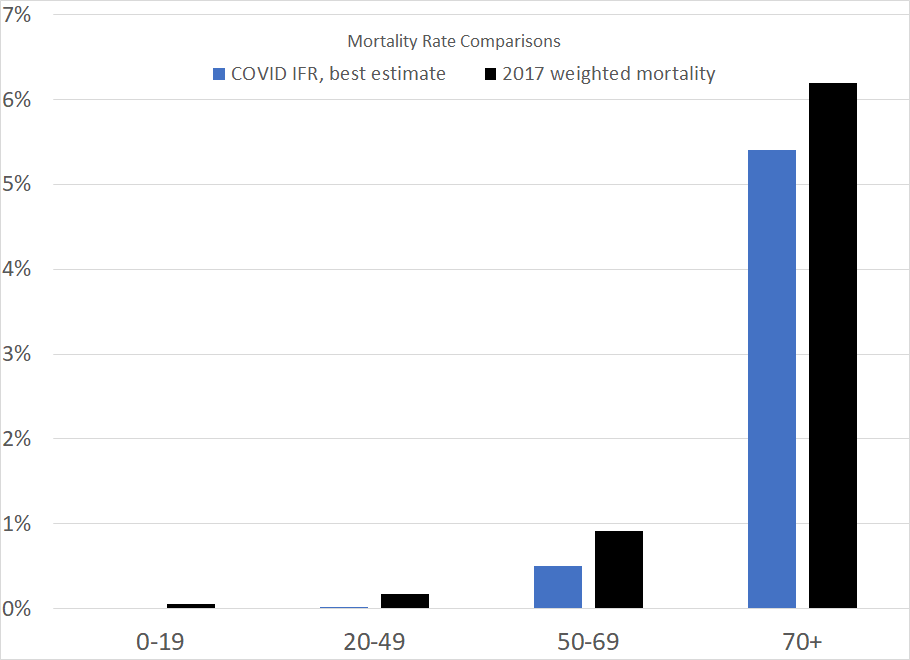
Using the Life Tables from 2017 (the last complete mortality info for the U.S.), and doing a weighted average of mortality, this is what regular mortality looks like:
So yay, regular mortality is higher than the infection fatality rate…. but now you can see where the idea of having double our usual mortality came from. For the oldest people, the infection fatality rate is very close to their normal mortality from all causes. If COVID’s effect is additive, then you’ve almost doubled the mortality for one year …. IF everybody gets infected with the disease and IF the IFR holds constant.
I will be sure to be revisiting this, as I just wrote an article for publication where part of it involved a mortality comparison between various pandemics. The age footprint for the Spanish flu was very different from what we’re seeing from COVID.
Herd immunity at what level?
I have to put dates on things, and you’ll see why.
22 September – MIT Tech Review: A city in Brazil where covid-19 ran amok may be a ‘sentinel’ for the rest of the world
What happens when a major city allows the coronavirus to rage unchecked?
If the Brazilian city of Manaus is any answer, it means about two-thirds of the population could get infected and one person in 500 could die before the epidemic winds down.
More than one person in 500 dies in a normal year in the U.S. [Indeed, almost 1% of the U.S. population dies in a year, in recent years.]
I’m getting annoyed by this sloppy wording. One person in 500 (that is, 0.2%) could die due to COVID. Plenty of people will die due to other things.
During May, as the virus spread rapidly in Manaus, the equatorial capital of the state of Amazonas, dire reports described overwhelmed hospitals and freshly dug graves. Demand for coffins ran at four to five times figures for the previous year. But since hitting a peak four months ago, new coronavirus cases and deaths in the city of 1.8 million have undergone a rapid and unexplained decline.
Yes, isn’t it funny how it doesn’t seem one can do much with respect to the onslaught of COVID…. but that once it burns through, it’s burned through.
Now a group of researchers from Brazil and the United Kingdom say they know why—so many people got infected that the virus is running out of hosts.
No kidding.
In a report posted to the preprint server medRxiv, a group led by Ester Sabino, of the Institute of Tropical Medicine at the University of São Paulo, says it tested banked blood for antibodies to the virus and estimates that between 44 and 66% of the population of Manaus has been infected since the city detected its first case in March.
Okay, those are quite large error bars. If it were a presidential poll in the U.S., one may ask if they had polled only 10 people.
And now — why I need to put dates on everything… I started this post on 24 September, and….
27 September 2020: In Brazil’s Amazon a COVID-19 resurgence dashes herd immunity hopes
The largest city in Brazil’s Amazon has closed bars and river beaches to contain a fresh surge of coronavirus cases, a trend that may dash theories that Manaus was one of the world’s first places to reach collective, or herd, immunity.
When a large portion of a community becomes immune to a disease, its spread becomes unlikely.
….
Local authorities on Friday enforced a 30-day ban on parties and other gatherings, and restricted restaurant and shopping hours, a setback for the city of 1.8 million after the worst of the pandemic seemed to be behind them.In April and May, so many Manaus residents were dying from COVID-19 that its hospitals collapsed and cemeteries could not dig graves fast enough. The city never imposed a full lockdown. Non-essential businesses were closed but many simply ignored social distancing guidelines.
Then in June, deaths unexpectedly plummeted. Public health experts wondered whether so many residents had caught the virus that it had run out of new people to infect.
…..
Infectious disease specialist Dr. André Patricio Almeida, at Manaus’ Heitor Vieira Dourado Tropical Medicine Foundation, said cases are rising again mostly among younger, wealthier people who go to bars who show milder symptoms but often infect older relatives who need to be treated in hospital.
…..
“Something that became evident in our study – and that is also being shown by other groups – is that antibodies against SARS-CoV-2 decay quickly, a few months after infection,” one of its authors, Lewis Buss, said in a statement by the São Paulo research foundation FAPESP that accompanied the paper.
So, in the above, I read that cases are rapidly increasing again. But, I haven’t heard confirmation that any of these are re-infections (maybe they are, of course) and, more to the point, I haven’t heard that deaths are up again.
Hmmmm.
We have seen a second wave of cases, but the deaths aren’t really following that closely.
Other cities should be cautious about drawing conclusions from Manaus since, among other factors, it has a fairly young population. Just 6% of citizens there are over 60, according to Brazil’s Institute of Geography and Statistics. In New York City, that figure is around 16% and for the US overall, it’s 20%. Elderly people have a much, much higher risk of dying if they catch the virus than younger people.
The Brazilian figures do suggest just how many people in one place could get infected as the virus spreads—a concept known as the attack rate. Were two-thirds of the US population to be infected, the virus could easily claim more than 500,000 American lives, mostly among the elderly. That’s in line with early projections for worst-case scenarios and with recent events on the ground. The US today surpassed the grim record of more than 200,000 deaths attributed to the virus. Tens of thousands of people are still being infected daily.
Originally, the worst-case scenario was estimated at 2 million extra deaths in the U.S., which would be a doubling of the normal rate. 500,000 is obviously also bad, but the extra number seems to be settling around 10% extra, not 100% extra.
The paper the above reporting on is here: COVID-19 herd immunity in the Brazilian Amazon, and I see where the large range of exposure comes from:
In June, one month following the epidemic peak, 44% of the population was seropositive for SARS-CoV-2, equating to a cumulative incidence of 52%, after correcting for the false-negative rate of the antibody test. The seroprevalence fell in July and August due to antibody waning. After correcting for this, we estimate a final epidemic size of 66%.
The lower number is based on actual testing, and the higher number comes from correcting for false negatives and that their testing sample was not representative of the full population.
AI Doesn’t Help With Shitty Data
MIT Tech Review: We’re not ready for AI, says the winner of a new $1m AI prize
You would think with a title like that, this interview with Regina Barzilay, the first winner of the Squirrel AI Award, would have nothing to do with COVID.
But it does.
Finally, why has AI not yet had much impact on covid-19?
AI is not going to solve all the big problems we have. But there have been some small examples. When all nonessential clinical services were scaled down earlier this year, we used an AI tool to identify which oncology patients in Boston should still go and have their yearly mammogram.
But the main reason AI hasn’t been more useful is not the lack of technology but the lack of data. You know, I’m on the leadership team of MIT’s J-Clinic, a center for AI in health care, and there were lots of us in April saying: We really want to do something—where can we get the data? But we couldn’t get it. It was impossible. Even now, six months later, it’s not obvious how we get data.
There have been so many deficiencies in COVID-related data that have become extremely obvious this year. People were creating dashboards of case counts and even mortality… and those of us who are actually subject-matter experts on what the data are supposedly showing (as opposed to SMEs on setting up pretty dashboards) realized a lot of these displays were bullshit.
I’ve already written about this twice on STUMP: A big lesson for data people: GET SOME STANDARDS
I have been driven nuts this year by poor data practices, even poorer modeling practices, and then decision-making purportedly driven by these two piles of trash. And then because of the big problems with the data and the models, the decision making becomes totally divorced from even fixed data and models.
…..
I do follow ASOP 23 when I’m dealing with data in my posts. I tell you where I got the data from, I let you know if I see problems with the data, and I let you know if there are aspects of the data I don’t understand.I don’t just pull stuff out of my ass and point to my credentials.
ASOP 23 is free to anybody dealing with data, and it is full of great advice.
The way you build up credibility is through practices such as these.
The difference between actuaries ignoring ASOP 23 and other data-using people not following its advice… actuaries can get expelled from the actuarial societies, and their credentials stripped. Poor data practices have been behind actuarial malpractice lawsuits.
I have found, in the long run, that if you want your reputation built up for solid quantitative analysis, you really need to follow standards such as these.
SO.
DO.
IT.
Go to the post for the Shia LaBeouf gif.
The other post on COVID-related issues was Mortality with Meep: COVID-19 Deaths and the Importance of Dates. When something is reported is meaningful only if we know when it actually occurred.
It is difficult to do meaningful analysis on COVID-related data when there are so many crucial missing pieces of info. The media report the number of “new” deaths, and the way they do it can end up with negative reported new deaths. Those of us who’ve had to deal with financial reporting know how sometimes you have to back out an item in an income statement, and it will be a negative though it literally doesn’t make sense.
(As an aside, once upon a time I thought up the fab actuarial fiction title of “Night of the Living Death Benefits”, but I suck at writing fiction.)
In any case, having had a little experience with AI, it really is not good at dealing with novel situations, and there are loads of things that humans are better at figuring out than algorithms driven by statistical models.
AI can’t get you past the garbage in/garbage out problem.
Covid Stories
Wired UK: China has almost eliminated Covid-19. What can the world learn?
Slate: Johnson & Johnson Starts Phase 3 Trial for Single-Dose Coronavirus Vaccine
CDC issues Halloween 2020 guidelines, color-coded COVID-19 risk map
Ars Technica: Trump may reject FDA’s stricter regulations for COVID-19 vaccine
The Economist: The covid-19 pandemic is worse than official figures show
NYT: As Virus Cases Surge in Europe, Hospitalizations Lag. But for How Long?
NYT: Novavax Enters Final Stage of Coronavirus Vaccine Trials
The Verge: Averting a COVID-19 vaccination crisis will take careful communication
The Economist [free content]: Tracking covid-19 excess deaths across countries – originally posted July 15, but updated regularly
UPI: Researchers find wide variance in accuracy of COVID-19 antibody tests
John Bury: Covid-19: Preface & Chapter 1
American Institute for Economic Research: A Primer for the Media on Viruses, Vaccines, and Covid-19
Video with Max Rudolph: Actuarial Implications of COVID-19
Think Advisor: 50 States of New Summer COVID-19 Wave Death Data, Plus D.C.
Enjoy!